Table of Contents
Introduction
Pneumonia is a severe respiratory infection or illness, a condition that primarily affects the lungs, especially the tiny or little air sacs named alveoli. In a healthy and normal individual, these alveoli facilitate the exchange or swap of carbon dioxide and oxygen; nevertheless, with this disease, they become inflamed and can fill with fluid, pus, or cellular debris.
This fluid-filled blockage impairs the lungs’ ability to deliver oxygen to the bloodstream, leading to symptoms such as difficulty breathing, cough, fever, and chest pain. It can be generated by a variety of infectious agents, including bacteria (most commonly), viruses, fungi, or even parasites, and its severity can range from mild, “walking pneumonia” to a life-threatening illness, particularly in vulnerable or prone populations such as the elderly, very young children, and individuals with weakened immune systems.
Pneumonia
Pneumonia is an illness in the lungs caused by bacteria, viruses, or fungi. It causes the lung tissue to swell (inflammation) and may create fluid or pus in your lungs. Bacterial pneumonia is usually more intense than viral pneumonia, which often settles on its own.
It can affect one or both lungs. In both lungs is named bilateral, or double, pneumonia.
Symptoms and Causes
Symptoms of this illness depend on the cause. Signs can range from mild to severe. Newborn Babies, young kids, and older adults may have different symptoms.
Symptoms of bacterial pneumonia
Symptoms of bacterial can grow slowly or suddenly. Signs include:
- Cough with yellow, leafy, or bloody mucus.
- Very high fever (up to105°FF or 40.55°CC).
- Rapid breathing.
- Tiredness (fatigue).
- Chest discomfort and/or abdominal pain, particularly with coughing or deep breathing.
- Shortness of breath.
- Rapid heart rate.
- Sweating or chills.
- Loss of appetite.
- Confusion or altered mental state.
Symptoms of viral pneumonia
Signs of viral pneumonia usually extend over several days. You might have signs similar to bacterial pneumonia, or you might also have:
- Dry cough.
- Muscle pain.
- Headache.
- Excessive tiredness or weakness.
Symptoms in young children
Babies and newborns may not display any signs of this disease, or their symptoms may be distinct from those of adults, including:
- Fever, chills, general discomfort, sweating/reddened skin.
- Cough.
Problem breathing or fast breathing (tachypnea).
- Failure of appetite.
- Vomiting.
- Absence of energy.
- Restlessness or fussiness.
Symptoms you can look for in babies and young kids include:
- Snorting sound with breathing or noisy breathing.
- A reduced amount of pee or diapers that are less wet.
- Pale skin.
- Limpness.
- Crying more than usual.
- Problem feeding.

Symptoms of pneumonia in adults over 65
Grown-ups over 65 or those with weakened immune systems may have milder or less noticeable signs of this disease (for example, cough and shortness of breath). Signs of ongoing health requirements may worsen. Older grown-ups may experience:
- An impulsive change in mental state.
- Low appetite.
- Tiredness.
What causes pneumonia?
It can develop when the immune system attacks an infection in the tiny sacs of the lung (alveoli). It causes the lungs to swell and leak fluids.
Many bacteria, viruses, and fungi may generate infections that lead to disease. Bacteria are the most common cause in grown-ups, and viruses are the most common cause in school-aged kids. Common conditions that may lead to disease include:
- Common cold (rhinovirus).
- The flu (influenza virus).
- COVID-19 (SARS-COV-2).
- Human metapneumovirus (HMPV).
- Legionnaires’ disease.
- Human parainfluenza virus (HPIV).
- Pneumococcal disease.
- Mycoplasma pneumonia bacteria.
- Pneumocystis pneumonia.
- Respiratory syncytial virus (RSV).
What’s the distinction between viral and bacterial pneumonia?
It is an inflammatory response to an infection in the lungs. You can have distinct symptoms depending on the primary cause: a virus, bacteria, or fungi.
Bacterial pneumonia is more familiar and more potent than viral pneumonia. It’s more likely to need a hospital stay. Providers treat bacterial pneumonia with antibiotics. Viral pneumonia induces flu-like signs and is more likely to resolve on its own. You usually don’t need precise treatment for viral pneumonia.
Is Pneumonia Contagious?
Yes, it can be contagious, but the degree and mechanism of contagion depend mainly on the underlying cause of the infection.
Here’s a breakdown:
- How it Spreads: The microbes that generate pneumonia (bacteria, viruses, or fungi) are generally spread through respiratory droplets when an infected or contaminated individual sneezes, coughs, and talks. Another individual can then inhale these droplets, or they may land on surfaces and be picked up by hands, which then transmit the microbes to the nose, mouth, or eyes.
- Bacterial: The bacteria that cause this disease (e.g., Streptococcus pneumoniae) can be contagious. However, not everyone exposed or prone to these bacteria will develop pneumonia; many people may carry the bacteria in their upper or higher respiratory tract without symptoms, or develop a milder infection like bronchitis. The development of pneumonia often depends on an individual’s immune system and other risk factors.
- Viral: Viruses (such as influenza, RSV, and SARS-CoV-2, which causes COVID-19) are highly contagious and a prevalent cause of pneumonia. Viral pneumonia often spreads readily through respiratory droplets, just like the common cold or flu.
- Fungal: Fungal pneumonia is generally not contagious from person to person. It usually occurs when an individual inhales fungal spores from the environment (e.g., from soil or bird droppings).
- Aspiration: This type of pneumonia, caused or generated by inhaling food, liquid, or vomit into the lungs, is not contagious at all.
Types of Pneumonia
In essence, while the underlying infection may be transmitted, direct transmission of “pneumonia” itself is not straightforward. The contagiousness lies with the exact germ pushing the inflammation.
It is classified in several ways, primarily based on cause, route of infection, and extent of lung involvement.
Here are the main types:
I. Based on the Cause (Etiology)
- Bacterial:
- Most Common: This is the most prevalent type, often severe.
- Common Organisms: Streptococcus (pneumococcus) is the most frequent cause. Other common bacteria include Haemophilus influenzae, Staphylococcus aureus, and Mycoplasma (often causes “walking pneumonia”).
- Symptoms: Can come on suddenly with high fever, chills, cough with pus or rusty-colored mucus, and rapid breathing.
- Treatment: Antibiotics.
- Viral:
- Common: Viruses are a widespread cause, especially in children.
- Common Organisms: Influenza (flu virus), Respiratory Syncytial Virus (RSV), Adenovirus, Varicella-zoster virus (chickenpox), Measles virus, and SARS-CoV-2 (causes COVID-19 pneumonia).
- Symptoms: Often milder than bacterial pneumonia, starting like the flu with fever, dry cough, muscle pain, and headache. Can progress to shortness of breath.
- Treatment: Antivirals (if available for the specific virus) or supportive care. Antibiotics are ineffective.
- Fungal:
- Less Common: More likely in people with weakened immune systems or those exposed to large quantities of fungi in the environment.
- Common Organisms: Pneumocystis jirovecii (often seen in HIV/AIDS patients), Histoplasma capsulatum, Coccidioides immitis.
- Spread: Not contagious from individual to individual; acquired by inhaling fungal spores.
- Treatment: Antifungal medications.
- Aspiration:
- Cause: Occurs when food, liquid, vomit, or saliva is inhaled into the lungs, often due to swallowing difficulties (dysphagia), impaired gag reflex (for example, from stroke, alcohol abuse, or anesthesia).
- Spread: Not contagious.
- Treatment: Antibiotics to treat the resulting bacterial infection.
II. Based on Where It Was Acquired
- Community-Acquired Pneumonia (CAP):
- Definition: It acquired outside of hospitals or other healthcare facilities.
- Causes: Can be bacterial (most common, especially Streptococcus pneumoniae) or viral.
- Hospital-Acquired Pneumonia (HAP) / Nosocomial:
- Definition: Pneumonia that develops 48 hours or more after admission to a hospital and was not incubating at the time of admission.
- Causes: Often due to more drug-resistant bacteria in the hospital environment.
- Risk Factors: Patients on ventilators, those with compromised immune systems.
- Ventilator-Associated Pneumonia (VAP):
- Definition: A type of HAP that develops in patients who are on mechanical ventilation.
- Causes: Often aggressive, drug-resistant bacteria.
- Healthcare-Associated Pneumonia (HCAP):
- Definition: It acquired in other healthcare settings, such as nursing homes, dialysis centers, or outpatient clinics.
- Causes: Can involve drug-resistant organisms similar to HAP.
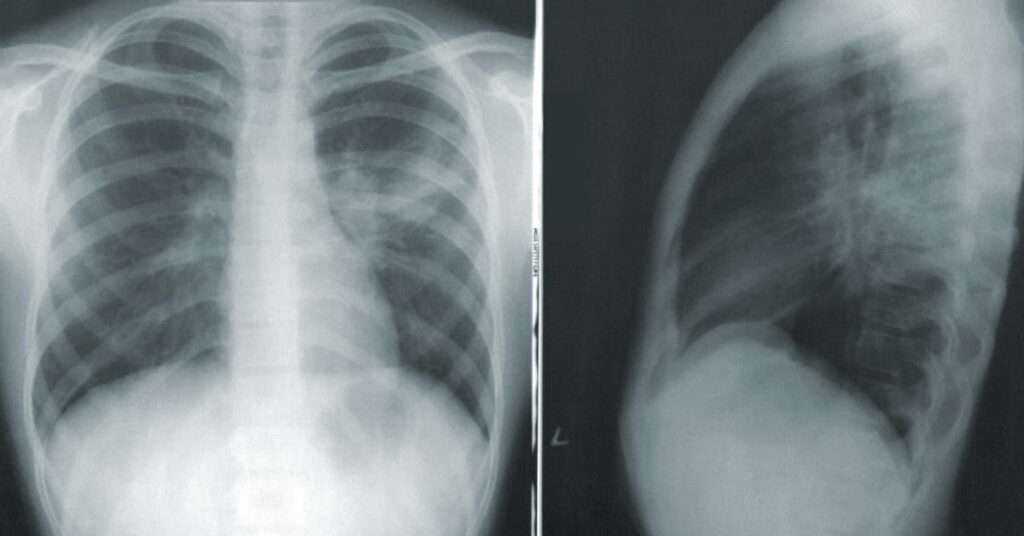
III. Based on Affected Lung Area (Radiological Pattern)
- Lobar Pneumonia: Affects a large, continuous section (lobe) of one or both lungs.
- Bronchopneumonia: Affects patches throughout the lungs, often involving the bronchi and bronchioles.
- Interstitial Pneumonia: Affects the interstitial spaces between alveoli, often seen in viral and atypical bacterial pneumonias.
Vaccine
There are effective Pneumonia Vaccines available that can significantly lower the chance of developing certain types of bacterial, as well as the severity of the disease if it does occur. These vaccines primarily target the most common bacterial cause of this disease: Streptococcus (pneumococcus).
In the United States, there are two main types of pneumococcal vaccines recommended by the Centers for Disease Control and Prevention (CDC):
- Pneumococcal Conjugate Vaccines (PCV):
- PCV13 (Prevnar 13): Protects against thirteen types of pneumococcal bacteria. It is routinely recommended for all infants and young children as part of their childhood immunization schedule. It is also recommended for some adults (65 years & older) and people with certain medical conditions.
- PCV15 (Vaxneuvance) and PCV20 (Prevnar 20): These are newer conjugate vaccines approved for adults. PCV20 protects against twenty types of pneumococcal bacteria. For adults 65 & older who have not previously received a pneumococcal conjugate vaccine, a single dose of PCV20 is recommended. If PCV15 is used, it should be followed by a dose of PPSV23.
- Pneumococcal Polysaccharide Vaccine (PPSV23 – Pneumovax 23):
- Protects against 23 types of pneumococcal bacteria.
- It is recommended or suggested for all adults 65 years & older, and for younger individuals (aged 2 to 64) with certain underlying health conditions (e.g., chronic heart, lung, liver, or kidney disease, diabetes, weakened immune systems, or smokers).
- Often given in sequence with a PCV vaccine for comprehensive protection in adults.
Who is Recommended for Pneumonia Vaccines?
- All Infants and Young Children: As part of routine immunization.
- Adults 65 years and Older: Routinely recommended.
- Individuals Aged 2 to 64 with Certain Medical Conditions:
- Chronic heart, lung, liver, or kidney disease
- Diabetes
- Weakened immune systems (e.g., HIV, cancer, organ transplant, chronic steroid use)
- Cochlear implants or cerebrospinal fluid (CSF) leaks.
- Sickle cell disease or other functional/anatomic asplenia
- Smokers
Important Considerations:
- Protection against Specific Strains: These vaccines protect against the most common and aggressive strains of Streptococcus. They do not protect against all types of this disease (e.g., viral, fungal, or other bacterial).
- Flu Vaccine is Also Crucial: Getting an annual flu shot is also very important, as influenza (the flu) is a common viral cause or origin of this disease and can weaken the respiratory system, making it more susceptible to bacterial pneumonia.
- Consult a Healthcare Provider: It’s always best to discuss whether the pneumococcal vaccine(s) are appropriate for you or your family associate with a healthcare professional, as recommendations can vary based on age, health status, and previous vaccination history.
Medication
The medication for disease largely depends on its cause, severity, and the patient’s overall health. Since bacteria, viruses, or fungi may cause pneumonia, the treatment approach differs significantly.
Here’s a breakdown of common medications:
I. For Bacterial (Most Common)
- Antibiotics: These are the primary and main treatment for bacterial. The choice of antibiotic depends on:
- Severity of Infection: Mild cases may be treated with oral antibiotics at home; severe cases require IV antibiotics in a hospital.
- Specific Bacteria: If the bacteria can be identified (e.g., through sputum culture), a targeted antibiotic is used.
- Patient Factors: Age, allergies, underlying health conditions, and whether the pneumonia was acquired in the community or a healthcare setting (which might imply drug-resistant bacteria) all influence the choice.
- Common Antibiotics:
- Macrolides: Azithromycin (Zithromax), Clarithromycin (Biaxin)
- Tetracyclines: Doxycycline
- Beta-Lactams: Amoxicillin (Augmentin), Amoxicillin-clavulanate (Augmentin), (Rocephin) Ceftriaxone
- Fluoroquinolones: Levofloxacin (Levaquin), Moxifloxacin (Avelox) (often utilized for more severe or resistant cases)
II. For Viral
- Antivirals: Antibiotics are ineffective against viruses. Treatment focuses on managing or controlling the specific viral cause if an antiviral is available.
- Influenza (Flu) Virus: Antiviral drugs like Oseltamivir (Tamiflu), Zanamivir (Relenza), Peramivir (Rapivab), or Baloxavir marboxil (Xofluza) can be used, especially if started early, to reduce the severity and duration of flu-induced pneumonia.
- SARS-CoV-2 (COVID-19): Specific antivirals such as remdesivir or oral Paxlovid may be used in hospitalized patients or those at high risk or chance for severe disease.
- Other Viruses: For many other viral causes, specific antivirals are not available, and treatment is primarily supportive.
III. For Fungal
- Antifungal Medications: Those are used to treat fungal pneumonia. The type and duration of treatment depend on the specific fungus & the severity of the infection.
- Common Antifungals: Fluconazole (Diflucan), Itraconazole (Sporanox), Voriconazole (Vfend), Amphotericin B (for severe infections).
IV. Supportive Care (Regardless of Cause)
These treatments help manage symptoms & support recovery:
- Pain Relievers/Fever Reducers: Over-the-counter medications like Ibuprofen (Advil, Motrin) or Acetaminophen (Tylenol) to manage fever and chest pain.
- Cough Suppressants/Expectorants: May be used to manage bothersome coughs, but typically with caution, as coughing helps clear the lungs.
- Oxygen Therapy: For patients ot people with low blood oxygen levels (hypoxemia), supplemental oxygen is administered, often via nasal prongs or a mask.
- Intravenous (IV) Fluids: To prevent dehydration, especially in hospitalized patients.
- Breathing Treatments: Nebulized bronchodilators may be used to open airways if bronchospasm is present.
- Respiratory Therapy: Exercises and techniques to help clear lung secretions and improve breathing.
Important Note: Self-medication for a disease is extremely dangerous. It requires a proper medical diagnosis and a tailored treatment plan from a healthcare professional. Always consult a doctor for diagnosis and management.
Pneumonia Supportive therapy
Here are the key components of supportive therapy:
- Rest:
- Purpose: Essential for the body to conserve energy & direct its resources towards fighting the infection and healing.
- Guidance: Patients are advised to get plenty of sleep & avoid strenuous activities until fully recovered.
- Hydration:
- Purpose: Helps to thin mucus in the lungs, making it easier to cough up & clear. Prevents dehydration, especially with fever and rapid breathing.
- Guidance: Drink plenty of fluids like water, clear broths, herbal teas, or electrolyte solutions. Intravenous (IV) fluids may be necessary for hospitalized patients or for those unable to drink enough fluids.
- Oxygen Therapy:
- Purpose: Addresses hypoxemia (low blood oxygen levels) resulting from impaired lung function because of inflammation & fluid in the alveoli.
- Guidance: Administered via nasal cannulas, oxygen masks, or in severe cases, through mechanical ventilation, to ensure adequate oxygen delivery to tissues and organs.
- Pain and Fever Management:
- Purpose: Relieves discomfort from fever, headache, muscle aches, & pleuritic chest pain (sharp chest pain with breathing).
- Guidance: Over-the-counter medications like acetaminophen (Tylenol, Paracetamol) or ibuprofen (Advil, Motrin) are commonly used.
- Cough Management:
- Purpose: While coughing helps clear secretions, a severe, unproductive cough can be exhausting.
- Guidance: Mild cough suppressants may be used if the cough is debilitating, but generally expectorants (like guaifenesin) are preferred to thin and loosen mucus, facilitating productive coughing. Avoiding irritants, such as smoke, is also key.
- Nutritional Support:
- Purpose: Ensures the body receives adequate calories and nutrients to fuel the immune response and recovery.
- Guidance: Patients should try to eat small, frequent, nutritious meals. For very ill or intubated patients, enteral (tube feeding) or parenteral (IV feeding) nutrition may be required.
- Respiratory Therapy / Chest Physiotherapy:
- Purpose: Helps clear lung secretions, improve lung expansion, and prevent complications like atelectasis (collapsed lung).
- Guidance: Techniques include deep-breathing exercises, incentive spirometry, postural drainage, chest percussion (clapping on the chest), and vibration. These are especially important for hospitalized patients.
- Avoidance of Irritants:
- Purpose: Prevents further irritation to already inflamed airways.
- Guidance: Avoid smoking, secondhand smoke, air pollution, and other respiratory irritants.
- Monitoring:
- Purpose: Continuous assessment of vital signs (temperature, respiratory rate, blood pressure (BP), heart rate, oxygen saturation) & clinical status to detect worsening or complications.
- Guidance: Regular checks by healthcare providers are crucial, with appropriate diagnostic tests (e.g., chest X-rays, blood tests) as needed.
Supportive therapy provides the foundation for recovery, allowing the body’s natural defenses and specific antimicrobial treatments to work most effectively against the pneumonia.
Conclusion
It is an illness in the lungs caused by bacteria, viruses, or fungi. Pneumonia causes the lung tissue to swell (inflammation) and may create fluid or pus in your lungs. Bacterial is usually more intense than viral, which often settles on its own.




